Replacement Lens Options
Before intra-ocular lenses (IOLs) were developed, people had to wear very thick eyeglasses or special contact lenses to be able to see after surgery. Now with replacement lens options, several types of IOL implants are available to help people enjoy improved vision.
How IOLs Work
Like your eye’s natural lens, an IOL focuses light that comes into your eye through the cornea and pupil onto the retina, the sensitive tissue at the back of the eye that sends images through the optic nerve to the brain. Most IOLs are tiny and made of a flexible, foldable material.
There are many different IOL options that correct specific vision problems, so it’s important to know which lens option is best for you. Like lenses of eyeglasses, your IOL will contain your appropriate prescription to give you the best vision possible. Before surgery, your eyes are measured to determine your IOL prescription then you and Dr. Youssef will compare options to decide which IOL type is best for you. If you have astigmatism, Dr. Youssef will discuss toric IOLs and related treatment options with you.
Glasses may still be needed by some people for some activities and the type of IOL implanted will affect how you see when not wearing eyeglasses. There are premium IOL options that may reduce your need for eyeglasses. In certain cases, cost may be a deciding factor for you so it’s important to understand all your options.
Which Lens Option is Right for You?
Astigmatism? Not a problem for Toric IOLs
Most people with cataracts want not only to have clear vision after cataract surgery, but freedom from glasses too. One thing that can prevent that from happening is residual astigmatism after surgery. Astigmatism is very common before and after cataract surgery, enough to cause noticeably blurred vision without glasses. In the past, IOLs used in cataract surgery could not correct astigmatism and had to rely on a procedure during surgery that can correct some astigmatism (astigmatic keratotomy), but it’s limited and sometimes outcomes are unpredictable.
Thankfully for cataract patients with astigmatism, toric IOLs have been developed specifically to provide vision improvement for both eye conditions by more predictably correcting astigmatism during cataract surgery and preventing the need for glasses later on.
Monofocal IOLs
Monofocal IOLs are the most common type of lens implanted and have been used for decades. Monofocals can provide best corrected vision at either near, intermediate or far distances. People who choose monofocals usually have their IOLs set to see distant objects and use reading glasses for near objects (like a phone or book), however some opt to set their IOLs to see near objects and use glasses to see things at a distance. In any case, people who choose monofocals will need to wear either distance or reading glasses.
For patients who opt for monofocal IOLs but who want more independence from glasses, monovision may be the answer. Monovision is an alternative technique which involves implanting a lens in one eye which corrects for distance vision (typically the dominant eye) and in the other eye for near vision. It’s an optical trick and takes a week or two for the brain to adapt and effortlessly combine near and distance information allowing you to see both simultaneously. Monovision and can help reduce your dependence on reading glasses for near vision. People who regularly use computers or other digital devices may find this especially useful.
Monovision has been around for decades but today advancements in IOL technology can now offer a more coordinated visual experience called blended vision. Monofocal IOLs such as the TECNIS® Eyhance IOL (offered at PVSC) can increase the range of vision in each eye by correcting the dominant eye for intermediate to distance vision while the non-dominant eye is set for the near to intermediate range. Because of this overlap in the intermediate range, the brain is able to fuse the images from both the eyes seamlessly. Compare this to to traditional monovision in which each eye only sees near or far vision so the image disparity between the eyes is too high for the brain to perceive clearly.
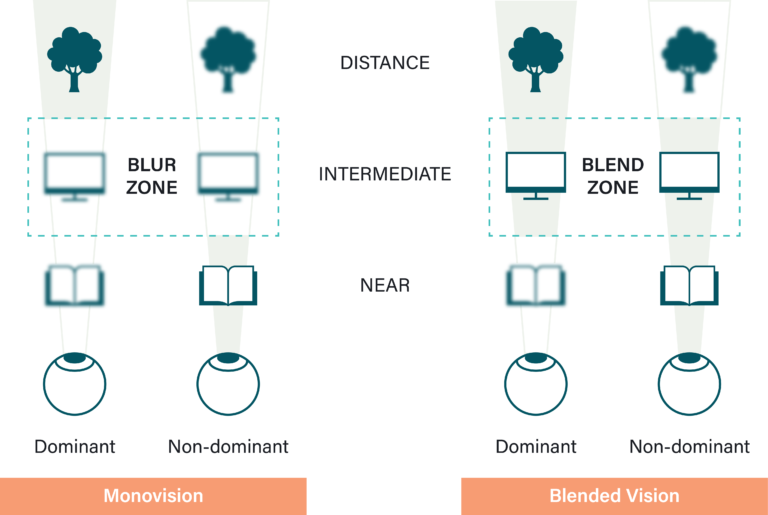
With blended vision, reading glasses may still be required occasionally but patients are much less dependent on them than traditional monovision patients.
Unfortunately, all currently developed options for correcting near vision may encounter night vision issues. While driving at night, patients can sometimes experience halos around sources of light, but it tends to improve with time as the brain adapts by suppressing these halos as noise. With blended vision, halos are caused by the nearsighted eye’s focus on the intermediate and near range. To resolve this issue if it persists, we recommend using prescription night driving glasses to allow both eyes to work together and give the best possible vision at night.
TECNIS® Eyhance IOL
TECNIS® Eyhance is a distance and intermediate vision monofocal IOL. It provides improved distance vision, both when you’re looking at things that are far away (like street signs) and at an intermediate distance (like a computer).
Instead of a lens with a single refractive power, the Eyhance lens slowly transitions from one refractive power on the edges of the lens and transitions seamlessly to a different refractive power in the middle. Instead of relying on monovision from two opposite lenses, this monofocal lens allows for a similar effect in one lens.
This IOL is not designed to give you reading vision, just to improve intermediate vision at 1 meter and up.
Multifocal IOLs
Multifocal IOLs are designed to provide additional focus points, allowing you to see clearly at different distances, near and far, reducing or eliminating the need for glasses or contact lenses. Multifocal IOLs enable not only clear distance vision and a comfortable reading distance but also good intermediate vision. Many patients with multifocal lenses do not need to wear glasses. This increased range of vision, however, comes at the cost of decreased sharpness of vision (ex. a person can read without glasses, but the words appear less clear than with glasses) and side effects like glare and halos around lights (mostly at night).
If you have very precise visual requirements like needing to focus on close-up work or if you perform a lot of night driving, multifocal IOLs might not be the best option for you and you may be more satisfied with monofocal IOLs.
TECNIS® Synergy IOL
TECNIS® Synergy IOL is a premium continuous-range-of-vision IOL and has high patient satisfaction rates and provides excellent vision.
Synergy IOL’s continued depth of focus offers the broadest range of vision of any IOL, including other popular premium IOLs like multifocal lenses and trifocals traditionally divided into different sections.
Because there’s no division between the different ranges of vision on the lens itself, the Synergy lens offers clear vision at all ranges with extra-sharp vision when looking at things up close. It also has superior contrast even in low light and can reduce or even eliminate the need for glasses.
Synergy was developed with violet-filtering technology that reduces the intensity of halos and starbursts for tasks like night driving, although it doesn’t completely eliminate them.
Light Adjustable Lens (LAL)
RxSight® Light Adjustable Lens™
The Light Adjustable Lens™ delivers superior visual outcomes that traditional IOLs cannot match. It’s the only FDA-approved IOL that can be customized after it’s been implanted in the eye. This means cataract patients can go about their daily activities to test their vision and fine-tune the lens even after surgery until they’ve achieved the visual outcome that suits them.
NEW! Light Adjustable Lens (LAL)
At PVSC, we’re excited to offer the latest in IOL technology – the Light Adjustable Lens™! This is the first and only lens that can be modified after surgery to optimize visual outcomes.
Calculating Your Lens Power
On the day of your assessment at PVSC, you’ll undergo an eye measurement to calculate your chosen replacement lens power. For more information on the replacement lens options we offer at PVSC, click here. These measurements are crucial to select the correct IOL power to ensure you achieve the best vision after cataract surgery.
How to Prepare for Your Assessment
If you wear contact lenses, remove them at least 1 week before your assessment. The longer you have them out, the more accurate your measurement will be.
Use artificial tears eye drops 4 times per day in both eyes starting 1 week before your assessment. These can be purchased from a pharmacy and you’ll continue to use them for at least two months after surgery (so they won’t be wasted, don’t worry!). A prescription for the surgery drops will be given at this appointment. You will also be given a schedule to follow for the eye drops.
Arrange with a friend or family member to join you during your appointment (only if you feel it might be necessary) and write down any questions you may have to discuss with us during your assessment.
To calculate your IOL’s power, there are two methods we use at PVSC: corneal topography and optical biometry.
Optical Biometry
Optical biometry is the current standard for IOL power calculations.
At PVSC, we use the LENSTAR LS 900® optical biometer which offers the best technology in IOL calculations. It’s non-invasive and provides us with highly accurate laser optic measurements for every section of the eye (from the cornea to the retina) in a single measurement. Optical biometry gives us useful measurements for every section of your eye, including the axial length (AL), the curvature of the cornea, corneal white-to-white (WtW) distance, and anterior chamber depth (ACD). This allows us to effectively and reliably calculate IOL powers for your surgery.
Corneal Topography
The cornea is the front transparent surface of the eye through which we see. Corneal topography is the technology we use for measuring the shape of the cornea. It’s a huge leap in eye measurement technology because it allows us to create a virtual image of your cornea (like a map) and from it, we can calculate the curvature of your cornea which is required to calculate the appropriate IOL for you.
To do this, a series of bright rings (called Placido rings) are projected onto the cornea and a camera takes a picture of the reflection. A computer analyzes the distortions in the reflections and turns it into a colour-coded map like the one below. Warm colors (red and orange) represent steeper areas and cool colors (blue and green) represent flat areas. This map gives us an overview of the corneal curvature as a whole and helps also detect abnormalities on your cornea. This normally requires multiple measurements with multiple machines but at PVSC we combine corneal topography with an optical biometer (the LENSTAR), improving workflow and convenience.
Corneal topography helps with calculations for IOLs, to assess astigmatism, and after refractive surgery to monitor changes in the eye. It provides invaluable information when evaluating pre- and post-surgical patients and can be used in many cases such as with patients who have had penetrating keratoplasty (PK), radial keratotomy (RK) or LASIK or especially for fitting of contact lenses (gas permeable) because the software helps design an appropriate lens, even recommending lens material, size, and design.
Important Notice For Post-Refractive Patients!
If you’re a patient who has undergone LASIK, photorefractive keratectomy (PRK), or radial keratotomy (RK), calculating your IOL power will be a challenge for any ophthalmologist because it is difficult to calculate accurate powers which makes surgery outcomes unpredictable. This happens due to:
Keratometric index error
When calculating your corneal power, we need to first measure the radius of curvature of your cornea (called the anterior corneal curvature). Once we know your radius of curvature, using a mathematical formula and the “keratometric index of refraction” (which is 1.3375), we can know your corneal power.
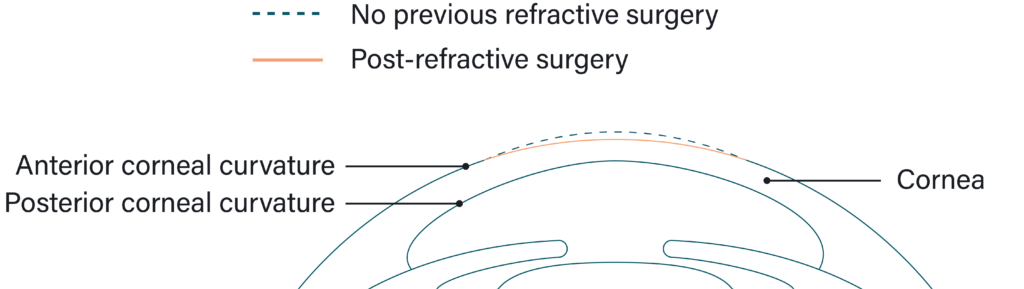
Our measurement devices are calibrated with the keratometric index of 1.3375. This is a standard number used for all patients. For eyes that have not undergone refractive surgery, this is fine because the shape of the cornea (the ratio between the anterior and posterior corneal curvature) is generally standard.
However in eyes that have undergone LASIK or PRK, the cornea is altered so the anterior corneal curvature has changed but the posterior curvature hasn’t. The ratio is disrupted and the standard keratometric index of 1.3375 no longer produces an accurate corneal power.
If you’re a patient who has had myopic correction, your corneal power might be overestimated and the IOL power underestimated so you’re likely to experience slight hyperopia after surgery.
If you’re a patient who has had hyperopic correction, your corneal power might be underestimated and the IOL power overestimated so you risk slight myopia after surgery.
Formula error
One of the most important measurements we need to know to determine the outcome of the IOL is the distance from the surface of your cornea to the surface of the IOL after it’s been implanted (called the effective lens position (ELP)). To calculate your ELP, we use mathematical formulas which incorporate your eye’s corneal power. As described above, unfortunately after LASIK or PRK, patients’ altered corneas are more difficult to measure making calculating the ELP challenging.
Ophthalmologists have methods to account for these errors and allow us to produce more accurate calculations. If available, your eye measurements from both before and after your refractive procedure will be used to calculate your IOL power. If this information isn’t known, we can still try to determine the refractive change using the power of your old contact lenses/eyeglasses.
At PVSC, we use state-of-the-art optical coherence tomography (OCT) (RTVue Total Corneal Power) to measure your corneal power and determine the IOL power calculation for cataract surgery on post-refractive surgery patients. This technology is much more accurate that traditional methods of calculating IOL power as it can directly measure the anterior and posterior surfaces of the cornea so no assumptions need to be made.
Please note the methods we use for lens calculation produce good refractive outcomes for post-refractive patients, but refractive surprises can still occur. We take many factors into consideration yet IOL power calculation is challenging. There’s a chance our refractive target may be missed so your postoperative results may differ from what was expected.
We offer bilateral same-day cataract surgery, a popular option for many patients. However, because of the inaccuracy of the calculations of IOL power for post-refractive patients, we do cataract surgery on one eye at a time with at least 2 weeks between in order to monitor the results of the first eye and adjust the IOL measurements for the second eye (if needed).
